
A recent report from the National Audit Office (NAO), titled ‘Progress in Preventing Cardiovascular Disease’, has brought renewed attention to a critical public health issue that continues to cost the UK billions: cardiovascular disease (CVD). Despite being one of the most preventable causes of death, CVD still places immense pressure on both the healthcare system and the wider economy. The NAO highlights NHS Health Checks as a key preventative strategy – yet, the system is currently falling short of its potential.
At Health Diagnostics, we welcome the NAO’s conclusions and offer our reflections and evidence-based insights into how the potential of the NHS Health Check can be realised and optimised These insights derive from over a decade and a half’s experience of supporting health check programmes across the UK.
NHS Health Checks: A Strong Case for Value for Money
The first thing the report highlights is the fact cardiovascular disease is a major avoidable cause of death that costs billions to the economy. The authors note that:
‘NHS Health Checks are the government’s key means for identifying and supporting people at risk of CVD who are not routinely identified by primary care. Given the costs of CVD to the healthcare system and the wider economy, Health Checks have potential to deliver value for money.’
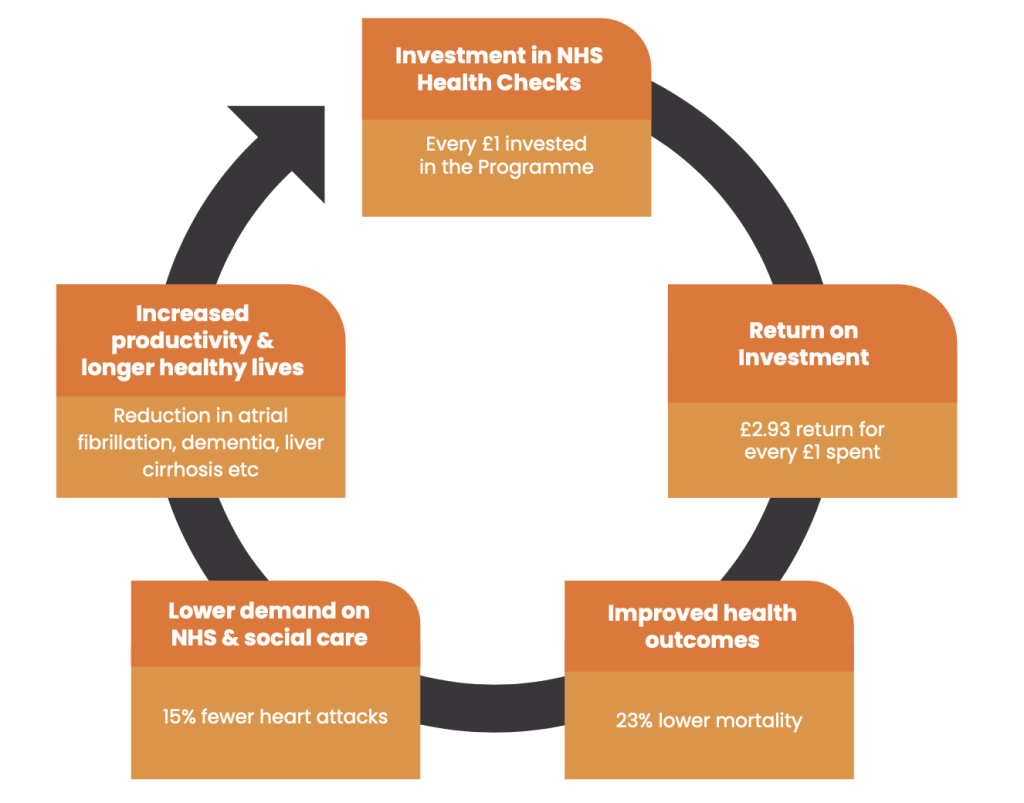
Given these vast costs, NHS Health Checks have significant potential to deliver value for money. Indeed, Health economic modelling published by the Department of Health and Social Care (DHSC) indicates that for every £1 spent, the programme delivers a £2.93 return on investment – through improved health outcomes, reduced demand on healthcare services, lower social care costs and increased productivity.
The strength of this case is further underpinned by a 2024 landmark study published by the National Institute for Health and Care Research. This real-world evaluation that drew on UK Biobank data from 48,602 individuals found that those who received an NHS Health Check had:
- 23% lower mortality over a 9-year follow-up
- Lower incidence of heart attack, dementia, and liver cirrhosis
- Higher diagnosis rates of diabetes, hypertension, and high cholesterol—denoting the opportunity to intervene early
These outcomes demonstrate how NHS Health Checks offer more than just short-term potential; they deliver long-term population-level benefits when implemented effectively.
Community-Based Models: Reaching Those Most in Need
Our work with Imperial College London, published in BMC Health Services Research, confirms that community-based outreach services, particularly when supported by Health Diagnostics’ technology, are effective at reaching underserved groups, including younger, more deprived, and ethnically diverse populations. These are the people often missed by traditional primary care routes.
Our own experience, supported by case studies like that of Medway Council, shows people’s risk of CVD can significantly drop within 12 months of a check. Medway Council Public Health oversees Medway’s NHS Health Check Programme and delivers the checks via GP practices, innovative community outreach and digital channels. It has partnered with us since 2020 to address challenges such as health inequalities, budget constraints and inefficient workflows. An observational analysis found that Medway’s community outreach approach led to a 10.5% reduction in CVD risk scores within a year (p<0.0001), compared to just 0.002% in a matched GP-based cohort (p=0.2526). This highlights the effectiveness of community outreach teams using Health Diagnostics’ system to drive meaningful health improvements – achievements not always mirrored in conventional clinical settings when the systems in use are not specialised and configured to support the delivery of motivational NHS Health Checks capable of truly inspiring lifestyle change.
These observations reflect findings from the BMJ Rapid Review Update (2022) of evidence relating to the NHS Health Check, which found that opportunistic and community-led delivery models can boost attendance, particularly among men and individuals from high-deprivation backgrounds.
Our conclusion: We strongly agree with the NAO’s assessment. Community-based provision is not an optional add-on, it is essential to unlocking the full benefits of NHS Health Checks.
Commissioning: A Fragmented and Costly Process
The NAO rightly criticises the current commissioning structure, where ‘each local authority goes through its own lengthy tender/procurement processes.’ It also highlights that ‘DHSC and local governments have weak levers to encourage primary care or other services to deliver Health Checks.’ We fully agree. When every local authority independently manages its commissioning, the result is a significant duplication of effort – wasting both time and public money.
Whilst local authorities may have different populations and therefore subtly different requirements (e.g. to account for the various services that may be available in different localities), it is also true that a more efficient and standardised national commissioning model would save local authorities time and money, whilst ensuring that best practice is baked in by design. The solution developed by our team can be completely tailored to local needs, as well as delivering the requirements set out by the DHSC. In our experience, this is a key balance to strike if solution commissioning and deployment is to be effective and deliver results for the populations being served.
We fully recognise that, due to the extent of budget cuts to local government over recent years, the requirement from organisations like ours to deliver value-for-money is essential. We have a strong track record of delivering this value in a cost-effective way – often by doing things differently and implementing innovative technology and new ways of working. In our experience, the key to success is often reflected in how willing the public health teams are to open-up and question their prior assumptions about how health checks can, and should, be most effectively delivered. For example, just because data collection templates available within a GP surgery’s existing clinical system have always been used before to deliver health checks, it does not mean a ‘business-as-usual’ approach is going to realise the full potential of the programme and inspire individuals to implement lifestyle change. In this sense, the “weak levers” that the NAO refer to not only relate to the delivery of health checks, but also the lack of strong incentives for ensuring those checks are delivered in a way that genuinely inspires meaningful lifestyle change.
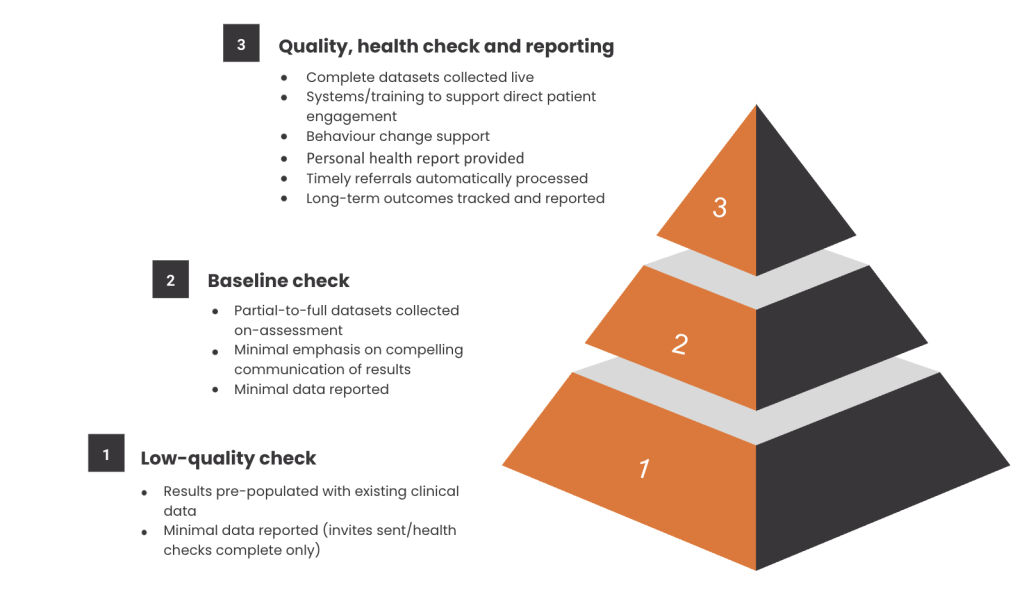
In terms of the data that gets reported back, when health checks aren’t delivered at high quality, this data will frequently cover just the bare minimum (i.e. number of invites sent, number completed). For those commissioning the programme in public health, such scant data offers no picture of the health trends that may be prevailing locally, as well as how they might be changing – for better or worse. Health authorities that Health Diagnostics support, however, have real-time access to comprehensive activity data across all types of providers. This can include long-term outcome data helping commissioners understand what has happened to people following their health check, 6-12 months down the line. It is this type of data that has allowed for the production of the Medway case study referred to above.
Health Checks Must Be More Than a ‘Tick-Box’ Exercise
The NAO report laments that:
‘In England, just under half of the annual eligible population attended a Health Check in 2023-24, and only 3% of local authorities delivered a Health Check for all their annual eligible population in 2023-24. This is not a satisfactory basis for delivering an important and potentially lifesaving and money-saving contribution to population health.’
This limited reach is deeply problematic, given the recent UK Biobank study has established that people who received NHS Health Checks experienced:
- Lower rates of: atrial fibrillation (irregular, often fast heart rate: 9% lower), dementia (19% lower), heart attack (15% lower), acute kidney problems (23% lower), liver cirrhosis (44% lower)
- A 23% reduction in overall mortality
Were local authorities delivering to more of their eligible population, these positive effects could be being felt even more widely. Yet, a persistent issue we see stakeholder scepticism about the programme’s value, often influenced by early, outdated reviews like the Cochrane analysis, despite the increasing evidence of positive impact (c.f. Tanner et al, 2022; McCraken et al, 2024; Robson et al, 2017 etc.). This attitude means engagement suffers: This scepticism can feed a self-fulfilling prophecy where low-quality delivery reinforces doubt, which in turn discourages investment or a focus on implementation. This fragmentation (misalignment of various local stakeholders) often leads to inertia, and ultimately to lower numbers of quality health checks being delivered.
It is very important that the health checks themselves are not deemed a ‘tick box exercise’ to collect a dataset, but rather as an opportunity to engage with individuals, support them to meaningfully understand their results, and show how changes can benefit them. Doing so effectively – as the latest research shows – will help people stay healthier for longer. Simply saying “you’re ‘normal’”, or “your results are fine” is not empowering or conducive.
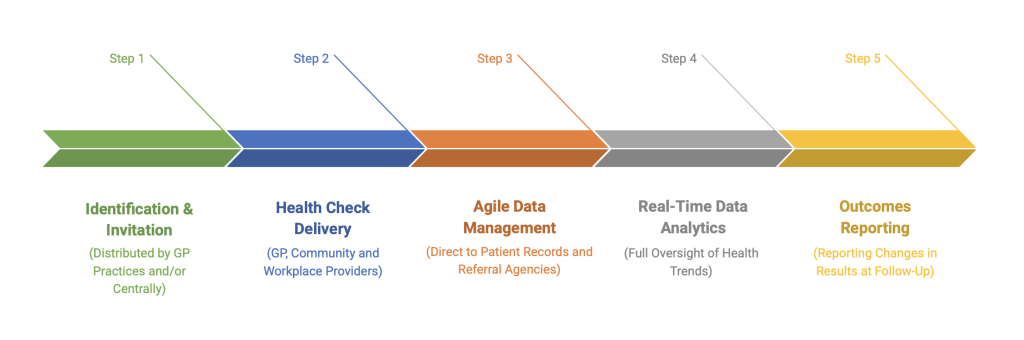
A practical hurdle in increasing uptake lies in the fact GP practices hold essential data to identify those who’d benefit from the NHS Health Check, however given the pressures on primary care, they may lack the time to focus on delivery. We have worked to bridge this gap by offering proven delivery models through a range of providers. Our ‘central invites’ function enables approved individuals working in public health teams outside of general practices to securely identify and invite patients into the Programme. This can allow for integration of GP-based with community care, as well as saving practices valuable time whilst ensuring effective implementation of the Programme.
Bridging the Data and Delivery Gaps
One of the most pressing NAO conclusions is that there is ‘no systematic targeting of those most in need,’ and limited data on what happens after a check. We anticipated this gap years ago, and have developed technology that enables real-time cohort identification, segmentation, and follow-up tracking.
Our system can:
- Identify priority groups which can be based on age, ethnicity, IMD, BMI, diabetes risk, and other factors
- Deliver tailored invitations (SMS, letter, phone)
- Provide comprehensive outcome tracking – from day of check, to 12 months post-intervention, and beyond.
This has enabled data-driven strategy for NHS Health Checks in areas like Medway, where real-time analytics have supported course corrections, engagement strategies, and evaluation of outcomes that go beyond tick-box metrics.
From Prevention Rhetoric to Prevention Policy:
The NAO report notes that:
‘DHSC will need to more effectively incentivise and target Health Checks if it is to achieve the difference it wants. Likewise, to embed the checks in a policy environment that promotes prevention, rather than treatment.’
Our view is that the power of the health check programme lies in its massive potential to inspire lifestyle change. The likes of Kent and Medway Councils are testament to how this can be achieved. Rolling out these hard-won learnings is key to sustained development. Currently, too much time and energy is being spent by local authorities ‘re-inventing the wheel’. A policy environment that looks closely at what is already working well, and encourages the spread and adoption of success, is essential.
Final Thoughts
NHS Health Checks are at a crossroads. The latest evidence confirms their ability to save lives, reduce strain on the NHS, and deliver exceptional value for money. Yet, fragmented commissioning, inconsistent quality, and limited uptake hold the programme back.
The path forward is clear: greater national coordination, community-centred delivery, digital integration, and a focus on outcomes over outputs. By aligning around what works – and investing in what matters – we can ensure NHS Health Checks become pivotal to a truly preventative, equitable healthcare system.
